KEY POINTS:
- Cyclops syndrome should be suspected if a post-ACL/R patient presents with progressive loss of knee extension, however, other causes of knee extension deficits should also be considered
- Confirmatory diagnosis is made using MRI
- Good patient outcomes can be achieved through surgical excision of cyclops lesion
Background & Objective
Cyclops lesion is a known complication of ACL reconstruction that occurs in up to 10% of ACL/R patients. It is known to cause knee extension deficits, which alters gait and knee mechanics. This potentially causes cartilage degenerative changes as early as one year post-op, making it a noteworthy complication.
A recent literature review was conducted to consolidate the available evidence regarding cyclops syndrome, cyclops lesions and its variants. It studied 47 relevant articles and summarised the latest research regarding the pathology, variants, etiological factors, diagnosis and management of cyclops lesions. Majority of these articles were case reports or case series. The key findings are as follows:
Pathology
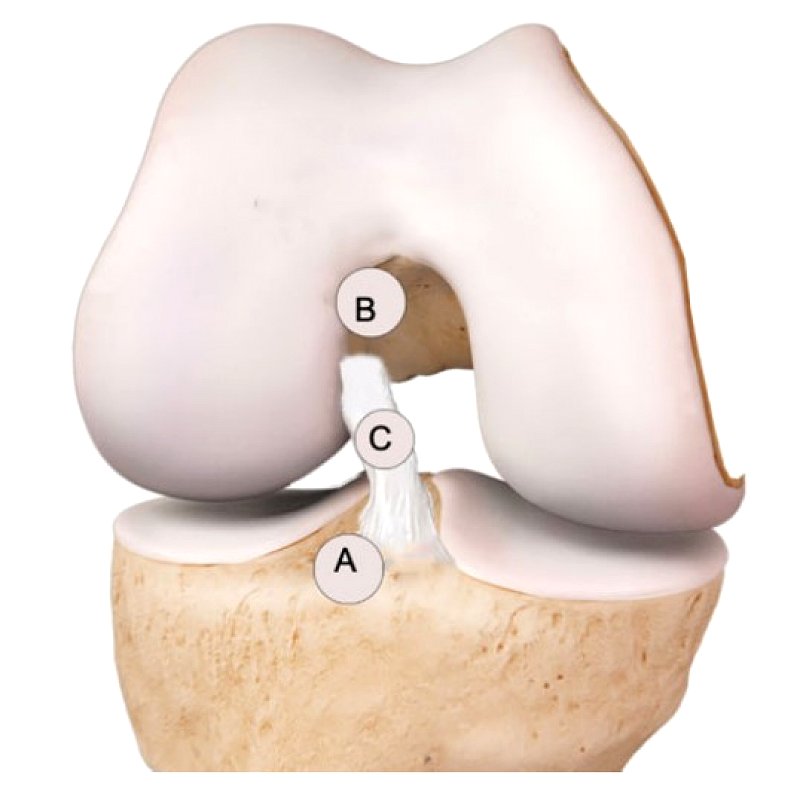
Cyclops lesion is a localised nodule of granulation tissue, also known as arthrofibrosis, that develops after an ACL reconstruction. It is specifically located anteriorly along the graft but can be further classified based on the location along the ACL.
A. Typical cyclops lesion: Located at tibial attachment of ACL (most common)
B. Inverted cyclops lesion: Located at femoral attachment of ACL
C. Atypical cyclops lesion: Located midsubstance of ACL graft
It has been proposed that cyclops lesions develop from the following:
- Avulsion pieces of bone from the tibial or femoral attachment of ACL
- Microtrauma causing granulation tissue formation
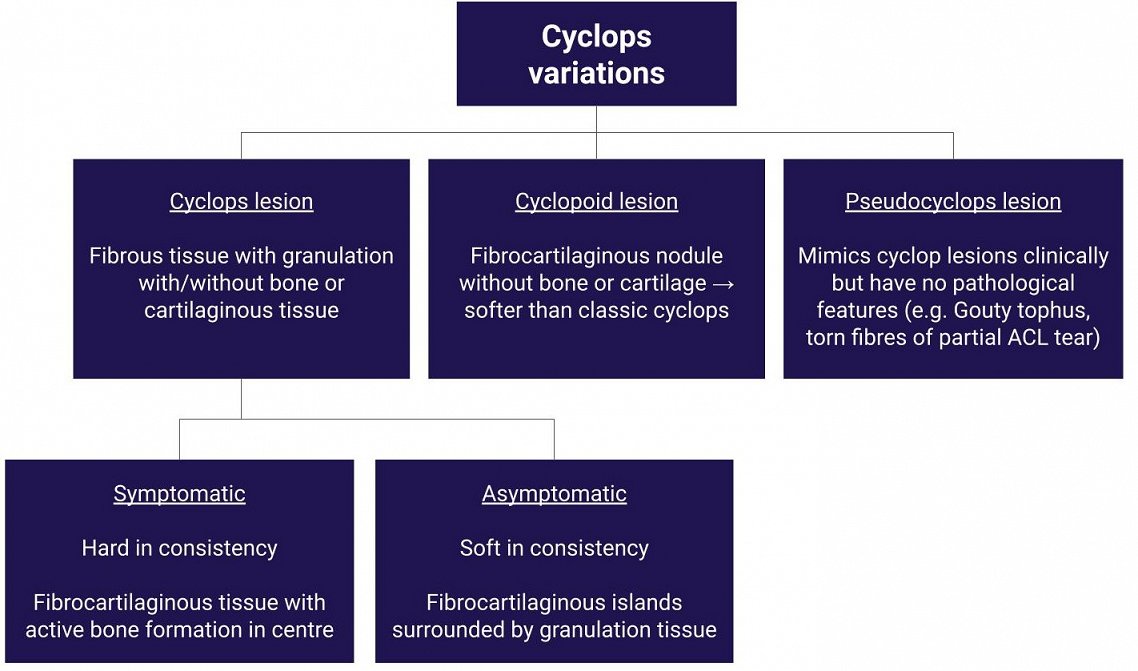
While 46.8% of all ACLRs reveal cyclops lesions during MRI, only 23% of these cyclops are symptomatic. Cyclops variations differ in their composition and this influences the presence of symptoms in patients. It has been shown that there is no correlation between the size of cyclops lesions and pain or other symptoms.
Etiological factors
The following were the risk factors identified for the formation of cyclops lesions:
- Female gender due to narrow notch
- Increased graft volume relative to notch size (e.g. double-bundle ACL/R, quads graft)
- Bicruciate-retaining total knee arthroplasty +/- ACL injury → cause injury to prosthesis and sharp edges of tibial bone island
- Anterior placement of tibial tunnel
- Bony avulsion of ACL from tibia/femur
- Persistent inflammation and hamstring muscle spasm
Clinical presentation
Cyclops syndrome is a term used to describe cyclops lesions with symptomatic loss of extension.
| Patient reported symptoms | Clinical observations |
|---|---|
| – Discomfort on walking/running/climbing stairs or when lying supine
– Anterior knee pain at terminal knee extension – Stiffness – Locking of knee – Crepitus |
– Progressive loss of terminal knee extension over 4 months post surgery (up to 20˚ loss)
– Pain and audible/palpable clunk at terminal knee extension – Rubbery at end-point of knee extension and bouncing back into flexion after attaining full extension – Joint line pain and tenderness – Temporary gains in extension, only to be lost at the next session – Poor gains in quads bulk |
While cyclops lesions are the 2nd most common cause of loss of extension post-ACL/R, there are other causes of extension deficits to consider and rule out:
- Hamstring contracture-related extension deficits
- Suprapatellar, intercondylar or capsular adhesions
- Arthrofibrosis
- Entrapment of patella tendon
- Meniscal tears
The diagnosis of cyclops lesions is confirmed through an MRI scan.
Management
Surgical excision of the lesion is recommended as it provides good prognosis and has shown to have low recurrence.
References:
Kambhampati, S. B., Gollamudi, S., Shanmugasundaram, S., & Josyula, V. V. (2020). Cyclops Lesions of the Knee: A Narrative Review of the Literature. Orthopaedic Journal of Sports Medicine, 8(8), 2325967120945671.